Epidemiology of Heart Failure in South Asian Countries
South Asian nations include India, Pakistan, Bangladesh, Bhutan, Sri Lanka, the Maldives and Nepal. The population of these countries accounts for about 25% of the world’s population, with approximations of each country shown in Figure 1. People of South Asian origin also constitute one of the largest ethnic groups in developed countries and the population is steadily growing.
In many South Asian countries, there are limited data from registries to establish an exact prevalence or incidence of heart failure (HF). According to the current universal definition, HF is a clinical syndrome with signs and symptoms secondary to a functional and/or structural cardiac abnormality corroborated by the elevation of natriuretic peptides (NP) or objective evidence of cardiogenic pulmonary or system congestion.1
If one were to use prevalence data from the US, in 2010 the prevalence was 1.87%, which would estimate the number of patients in India as of 2022 Indian population data at around 26.5 million.2 This number grossly underestimates the true prevalence because many South Asian countries, such as India, experience a ‘double burden’. This refers to the increase in non-communicable diseases (NCDs), such as hypertension, type 2 diabetes (T2D) and coronary heart disease (CHD), alongside the persistence of ‘traditional’ diseases, such as rheumatic heart disease (RHD).3

Although HF is predominantly thought of as a disease of the elderly, South Asian descendants have been shown to have a much younger age of initial presentation. Compared to European and developed countries, data from the Trivandrum Heart Failure Registry (THFR) in India have shown that HF presents almost 10 years earlier in age in Indians than in other ethnic counterparts, with a mean age of 61 years. The INTER-CHF study also showed a mean age of presentation of HF of 56 years in Indians, while the mean age of presentation in the US was around 72 years. These registries also revealed increased in-hospital mortality of almost 8.4% in THRF, compared to 4% noted in the Acute Decompensated Heart Failure National Registry (ADHERE) in the US.
When examining data from HF registries in developed nations, South Asian immigrants have also been shown to have significant differences in comorbidities when compared to individuals of other ancestries. Studies in many European and developed nations such as the UK, Canada, and the US have shown a younger age of HF presentation, a higher likelihood of having comorbidities of coronary artery disease (CAD) and diabetes, and more hospital readmissions.4,5 When looking at one small sub-analysis of a large ethnic population-based study in London (LOLIPOP), South Asians were found to have significantly higher BMI, fasting triglycerides, and lower HDL cholesterol concentrations compared to European counterparts.6 Altogether, this suggests a population with both a higher burden of comorbid risk factors leading to downstream HF, as well as a worse prognosis once the diagnosis is established.
Current estimates from 2014 show that the prevalence of HF in India ranges from 1.3 million to 4.6 million.7 As of 2006, Pakistan had an estimated 2.8 million citizens with a diagnosis of HF.8 Due to insufficient reporting, the total numbers are unknown in other South Asian countries, such as Bangladesh, Nepal, Bhutan, Sri Lanka and the Maldives. With the increased life expectancy and an increased prevalence of NCDs, these numbers are estimated to continue to rise exponentially within these countries.
Risk Factors for Heart Failure in South Asian Populations
Air Pollutants
Chronic exposure to air pollution is an important risk factor in the development of cardiovascular disease (CVD).9 Common pollutants include particulate matter, nitrogen oxides, sulphur dioxide, carbon monoxide, volatile organic compounds, ozone and heavy metals. Indoor and outdoor air pollutants have increased in many South Asian countries over the past 25 years. Of the top 30 cities with the poorest air quality in 2016, 17 were in South Asian countries.10 Continued urbanisation has led to increased air pollutants from vehicular exhaust and industrial activity in South Asian nations.11 Indoor pollutants have also risen within large urban centres. One of the reasons for increases in indoor pollutants is that 74% of South Asian households use solid fuels such as wood, dung or coal for cooking and heating.12,13 In the absence of a proper ventilation system in many households, the effects of particulate matter are further amplified. Although the exact mechanisms are unknown, indoor air pollutants are associated with increased atherosclerosis, increased coagulopathy, elevated inflammatory markers leading to myocardial remodelling, and altered autonomic tone which may confer risk toward cardiac arrhythmias. The downstream burden of rising air pollutant exposure to individuals who originate from South Asian nations may increase the potential risk for both CAD and the downstream risk of HF.
Coronary Artery Disease
CAD can result in angina, MI or other complications. Multiple epidemiological studies have shown that South Asian immigrants in developed countries have markedly increased rates of CAD compared to other ethnic groups.14 In addition, South Asians have also been shown to present earlier with more diffuse CAD compared to their white counterparts.15 Even when risk stratifying for NCDs that may accelerate CAD such as diabetes, South Asian patients demonstrate more advanced atherosclerosis with a higher number of vessels with ≥50% diameter stenosis on coronary CTA compared to white patients.16
There are mixed data regarding the luminal diameter of coronary arteries across ethnic populations. A retrospective observational study comparing South Asian and white patients who underwent cardiac catheterisation on the same day at the University of Pennsylvania demonstrated that South Asian patients displayed smaller proximal left anterior descending artery luminal diameters when normalised for body surface area. Further analysis from this study found this was despite South Asian patients presenting with lower LDL cholesterol compared to their white counterparts.17 Other studies, including one by MASALA (Mediators of Atherosclerosis in South Asians Living in America), have also shown that South Asians demonstrate an increased carotid intimal-medial thickness when matched to subjects in the MESA cohort (Multi-Ethnic Study of Atherosclerosis). Although the early and aggressive development of CAD is likely a multifactorial process that is still not well understood, these studies have shown that these factors likely accelerate the rates of HF in South Asian populations.
Diabetes
Diabetes can lead to various complications affecting the eyes, kidneys, nerves, and cardiovascular system. Diabetes and insulin resistance are major risk factors for increased morbidity and mortality in a multitude of CVDs, including CAD and HF. South Asian individuals have an up to 50% higher rate of prevalence of T2D compared to other ethnicities.
Diabetes may contribute to the development of cardiomyopathy. Major consequences of diabetic cardiomyopathy include cardiac remodelling, affected myocardial tissue perfusion, increased myocardial scarring, and disruption of myocardial energy metabolism.18 With these physiological changes, individuals with diabetes are more likely to develop HF at younger ages alongside more advanced forms of HF. By 2030, it is projected that approximately 120.9 million people of South Asian descent will be affected by diabetes (90–95% of these cases being T2D). This is projected to be double the number of people who will be affected in North America and Europe.19
Lifestyle changes and medications continue to be at the forefront of diabetes management, yet South Asian populations are less adherent to both these, leading to extremely poor glycaemic control compared to other populations. Some of the biggest obstacles to lifestyle modifications include lack of knowledge and cultural differences.20 Diet has also been a driving factor as many traditional meals are high in calories, carbohydrates and saturated fats, and low in fibre. As the diabetes epidemic continues rising within this region, HF may also become more evident.
Hypertension
Hypertension is a significant risk factor for various CVDs, including stroke, MI and HF. Hypertension, which WHO rates as one of the most important risk factors for premature death, exerts significant financial burdens in many South Asian countries. Recent meta-analyses of national registries within this region have shown the prevalence to be around 20–30%.21,22
The PURE study, which was conducted in urban and rural locations in 17 countries in Asia, Africa, Europe, and North and South America found that awareness and treatment of hypertension were extremely low in South Asian countries compared to other regions. The PURE study, which had a slightly older cohort with a mean age of 48.5 years, found that approximately one-third of the population studied from Bangladesh, Pakistan, and India were diagnosed with hypertension. Prevalence was highest in Bangladesh (39.3%), followed by Pakistan (33.3%), and lowest in India (30.6%). Among this study population, only 40% of individuals with hypertension were aware of their diagnosis, 32% of those individuals were treated, and only 13% showed adequate blood pressure control.23
Further analysis of demographic health surveys from India (2019–2021), Nepal (2016), and Bangladesh (2017–2018) have shown that hypertension is also prevalent in the middle and upper class populations within this region. Factors that have led to this trend include dietary indiscretion, sedentary lifestyles, pollution within large city centres, and the more common practice of using tobacco products.24 Although specific blood pressure targets based on racial/ethnic backgrounds have not been defined, earlier identification and treatment of hypertension should be pursued in this population to help prevent future HF.
Metabolic Syndrome
Metabolic syndrome is a cluster of interconnected metabolic abnormalities, including obesity, insulin resistance, dyslipidaemia (abnormal lipid levels), and hypertension. Individuals with metabolic syndrome are at increased risk of developing CVDs, T2D and other conditions. Metabolic syndrome is defined as someone who has three or more of the following risk factors: glucose intolerance, abdominal adiposity, elevated triglycerides, and HDL cholesterol levels, and is at the highest risk for the development of CVD.25
Multiple analyses from the landmark MASALA study have demonstrated that South Asians, specifically men residing in the US, have a higher amount of total abdominal adipose tissue, subcutaneous abdominal adipose tissue, and visceral adipose tissue, despite only mildly elevated BMI compared to other ethnicities. Given these data, South Asians with central adiposity are more likely to have abnormal metabolic profiles.26
When further investigating the metabolic profiles of individuals of South Asian descent, it has been shown that both men and women have lower levels of HDL compared to white individuals. Among those with the lowest levels of HDL are native, urban-dwelling Indians. Even when stratifying for social class and South Asian descendants living in developed parts of the world, it has been shown that hypertriglyceridaemia is more common in immigrant Indians and native Indians of higher socioeconomic class than their white counterparts.27 One reason hypothesised for this trend, which was shown in the INTERHEART study was that physical exercise was lowest in South Asians compared to other groups (6.1% versus 21.6%).28 A combination of all these aforementioned factors causes an imbalance in cardioprotective and cardiotoxic metabolisms which all lead to the early development of HF among South Asian descendants.29
Rheumatic Fever
Valvular heart disease is a leading cause of CV morbidity and mortality worldwide and RHD is the most common cause.30 RHD is a condition resulting from rheumatic fever, an inflammatory disease caused by untreated streptococcal infections. It primarily affects the heart valves, leading to valve damage and dysfunction, which can result in HF, arrhythmias, and other complications. RHD increases the risk of CVD, such as AF and HF.31 It is estimated that the number of children with RHD in South Asian populations currently ranges between 2.0 and 2.2 million.32 These numbers may still underestimate the impact of RHD as this condition occurs early on in childhood and there are limited surveillance programs among South Asian populations to obtain a true estimate. A recent genome-wide association study (GWAS) has shown that RHD has a genetic component. The risk of developing RHD in an individual with a family history of RHD is nearly fivefold higher than in an individual with no family history of RHD.33 This GWAS showed a major susceptibility locus for RHD in the human leukocyte antigen region, which is strongly associated with susceptibility to RHD in South Asians and Europeans.34 With rapidly rising populations and limited medical resources in rural areas of this region, the impact of early acquired diseases such as RHD will continue to play a significant role in these populations as they age and the prevalence of conditions such as HF will become more evident.
Smoking
There is a strong association with tobacco use and the development of HF, as well as the exacerbation of existing HF. The pathophysiology behind this association involves various mechanisms, including direct toxic effects, endothelial dysfunction, inflammation and impaired oxygen supply.35–37
Tobacco products, including smokeless tobacco and bidis/beedis, have become increasingly common in many South Asian countries with continued urbanisation of many areas within this region and a strong influence of family habits. In India, some studies have shown that smoking tobacco is common among school-age children and that approximately 20% of Indians smoke daily.38 Traditionally, many South Asian cultures consider smoking tobacco as taboo. Thus, another common practice, especially among South Asian women and young children, is the use of smokeless tobacco in the form of tobacco leaves. In one study of the large metropolitan city of Mumbai, the prevalence of tobacco use was estimated to be around 57.5% in women, almost solely in the form of smokeless tobacco. The same study found the prevalence among men to be approximately around 69.3%, with 45.7% of them reporting using smokeless tobacco.39
Another challenge many South Asian countries face is the prevalence of bidis, which are conical-shaped bundles of coarsely grounded tobacco costing less than one-fifth of the cost of cigarettes. Given their low cost, bidis are commonly popular among the lower class in India, Bangladesh and Sri Lanka. Taxation of bidis has also been an issue as the low cost of production has led some small manufacturers to exploit small companies to avoid taxes completely within this region.40 In South Asia, Bangladesh, India and Pakistan had the highest prevalence of tobacco consumption (43.3%, 34.6% and 19.1%, respectively).41 Despite increasing government taxation on tobacco in many South Asian countries, tobacco products continue to be one of the leading risk factors for the HF crisis.
Genetics and Unique Biomarkers
Monogenetic and Polygenetic Markers
Hypertrophic cardiomyopathy (HCM), characterised by left ventricular hypertrophy, is the most inheritable genetic cardiomyopathy and a common cause of sudden cardiac death and progression to HF in all ages.42 Mutations seen in MYBPC3, a thick filament in cardiac muscle protein that regulates cardiac contractility, are associated with approximately 40% of all HCM cases. Of interest, an autosomal dominant South Asian specific variant, a polymorphic 25-base pair deletion in intron 32 of MYBPC3, is present in 4–6% of SA individuals or equivalent to ~100 million people worldwide. This risk allele leads to late-onset left ventricular dysfunction, hypertrophy and HF with multiple forms of cardiomyopathy.43
Studies looking at the frequency of sarcomeric gene polymorphisms with left ventricular dysfunction in patients with CAD have shown that having MYBPC3 polymorphism compared to other gene mutations is associated with an increased risk of left ventricular pathological remodeling.44 Furthermore, additional studies looking at whole genome sequencing in patients in the US presenting with MI before the age of 65 have shown that having an increased polygenic score along with hereditary risk factors led to a 3.8-fold odds of early onset MI.
Currently, there are no clinical biomarkers that can help identify individuals with high polygenic scores, and the majority of the studies that have analysed these scores have shown that the prognostic importance remains highest in white patients. Despite this, Khera et al. showed in their genome sequencing study that a high polygenic score has prognostic utility across all races, but requires the inclusion of a more diverse population of genetics.45 Given that identifying individuals with high polygenic scores at an earlier age can help mitigate early onset heart disease, further studies looking at the genome of South Asian descendants will be of great importance.
Lipoprotein(a)
When looking at conventional risk factors for CHD, dyslipidaemia is a strong independent factor that is disproportionately found in South Asian descendants compared to other ethnicities. When specifically looking at the lipid panel, South Asians are shown to have elevated levels of triglycerides, low levels of HDL cholesterol and elevated lipoprotein(a) [Lp(a)] levels. Lp(a) is a form of LDL that carries cholesterol to the cells in the arteries.46 Lp(a) is highly atherogenic and is associated with premature atherosclerosis in coronary, cerebral and peripheral arteries.47
The levels of Lp(a) in an individual are primarily genetically determined with South Asian descendants having higher levels than their white counterparts.48,49 This was shown in the analysis of INTERHEART populations, which demonstrated a strong relationship between elevated Lp(a) concentrations as a risk factor for MI.50 When comparing South Asian immigrants versus community dwellers, Bhatnagar et al. showed that levels of Lp(a) were similar in immigrants in west London and individuals living in the state of Punjab.51
Currently, new therapies are being studied to target lowering Lp(a) levels through antisense oligonucleotides, small-interfering RNA-based therapies, and gene editing, which would help lead to a reduction in atherosclerotic cardiovascular diseases (ASCVD). Genome-wide association studies have been able to link single nucleotide polymorphisms to elevated levels of Lp(a), with >90% of variance controlled by the LPA gene. Two phase III clinical trials with a focus on lipoprotein(A) are currently underway. Lp(A) Horizon (NCT04023552) is focusing on the use of pelacarsen to reduce cardiovascular risk in patients with cardiovascular disease and elevated Lp(A). Additionally, the OCEAN(a) trial (NCT05581303) will focus on the use of olpasiran to reduce cardiovascular events in patients with atherosclerotic cardiovascular disease and elevated Lp(A).52
Management
HF, which affects approximately 26 million people worldwide, is estimated to have cost $102 billion in treatment worldwide in 2012.53,54 Costs incurred by HF care included direct costs (expenditure on hospital and physician services, drugs, and follow-up) and indirect costs (due to lost productivity, sickness benefit, and welfare support). When comparing overall contribution to global HF spending, the US ranks at the top, spending about 28.4% of global costs, while South Asian countries only contribute about 1.1%, ranking the lowest in the world.2
The medical management of HF, particularly HF with reduced ejection fraction (HFrEF), has multiple large randomised controlled trials (RCTs) that have shown guideline-directed medical therapy (GDMT) can improve morbidity and mortality. Neurohormonal antagonists, including angiotensin-converting enzyme inhibitor (ACEI), angiotensin receptor blockers (ARBs), β-blockers, mineralocorticoid receptor antagonists (MRAs) and sodium-glucose cotransporter 2 (SGLT2I), have all been shown to have a significant improvement in the morbidity and mortality of the treatment of HFrEF. Many novel diabetic medications, including SGLT2I have been shown to have significant benefits in HF across the ejection fraction spectrum.
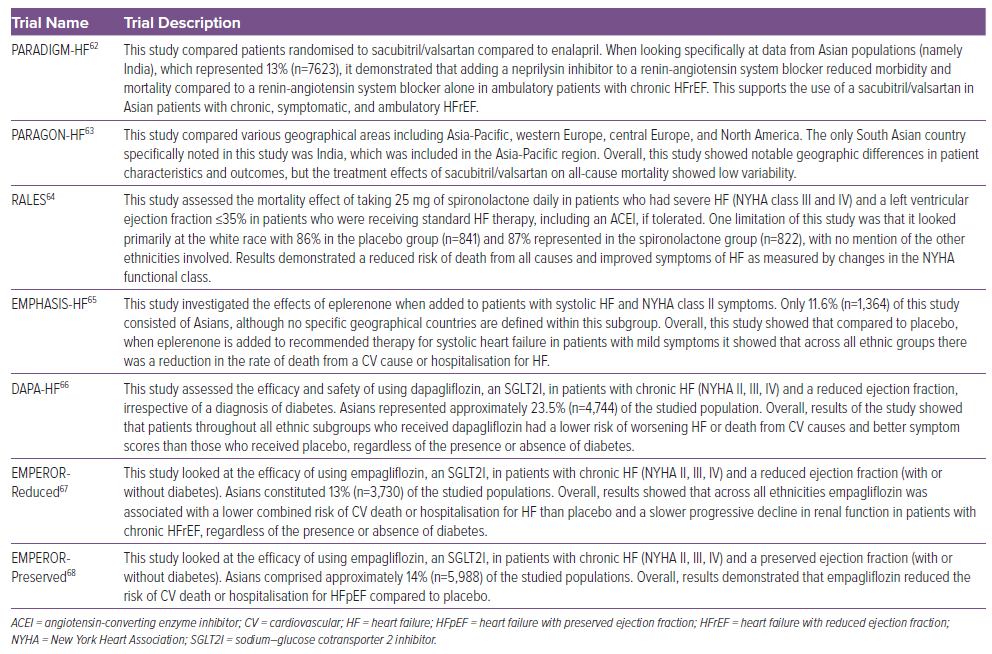
Few data are available to stratify these differences in lower-income countries. A recent meta-analysis of approximately 414 HF RCTs found that <15% of the participants were outside Europe and North America.55 Even with the drastic under-representation of South Asians in these landmark trials, there is no evidence to support the premise that these class I HF recommendation medications would be less effective in the South Asian population. These results are shown in Table 1.
Despite the knowledge of these novel therapeutic medical options, THFR reported the use of GDMT at discharge in 25% of its participants. Similarly, the Practice Innovation and Clinical Excellence (PINNACLE) registry in India, consisting of 15,870 outpatients with HF, aimed at cardiovascular quality improvement saw that only 29.6% of outpatients with HF were on both ACEIs/ARBs and β-blockers. One major finding from the PINNACLE registry was that the documentation of GDMT was higher in facilities with electronic health records compared to sites that did not have electronic records.56 Overall, though, lack of education on HF and medication costs were cited as some of the major reasons for the lack of GDMT.
Device therapy, specifically CRT, has also been shown to improve mortality and reduce hospitalisations in patients with a diagnosis of HF. The South Asian Systolic Heart Failure Registry (SASHFR) looked at a sample population of 471 patients on optimised HF medical therapy who met CRT implantation guidelines during a 2-year follow-up period after the initial diagnosis of HF. This study showed a clear superiority of CRT over optimal pharmacological therapy in the improvement of HF symptoms in South Asian populations. Despite this, only 24% of participants accepted to be implanted with a CRT device, with financial constraints being the main reason for refusing implantation of this device.57
As many of these new devices are not cost-effective and the number of patients with HF far exceeds the capabilities in many parts of the region; the mainstay of HF treatment must focus on GDMT, medical adherence and lifestyle changes.
Prevention
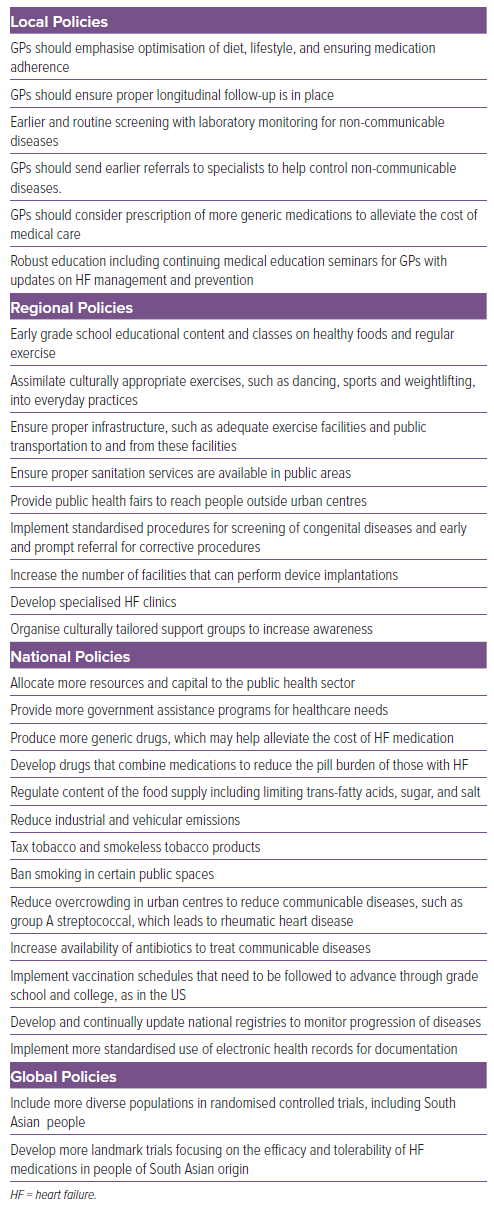
Despite the recent rising epidemic of HF among South Asian nations, we advocate a series of steps listed in Box 1 that may be taken at local, regional, national and global levels to help lessen the impact.
Discussion
As South Asian countries constitute one-quarter of the world’s population and are rapidly growing, the health burdens faced within these communities are important to highlight. Another key point is that South Asian descendants within industrialised countries are also facing an impending HF crisis compared to other races residing within these regions. South Asians in many developed countries have been shown to have higher rates of CHD and metabolic syndrome compared to other races. Risk factors that have led to this increased risk of CHD, other NCDs and, ultimately, HF include urbanisation, irregular timing of meals and assimilation of the traditional South Asian diets with the cuisine of developed nations.58 Although it has been noted that both immigrant and local South Asians are universally affected by the HF epidemic, no studies are available at this time to compare the two groups.
Despite the growing epidemic of HF within South Asians globally, many industrialised countries have begun the process of starting structured programmes and passing legislative laws to increase awareness. One such programme in the US included the SAHELI community-based participatory research study, which targeted underserved South Asian immigrants. This study showed that through an academic–community partnership model, focused on interactive group classes to increase awareness of physical activity, healthful dietary changes, stress management and longitudinal follow-up that ASCVD risk factors were mitigated.59
Similar actions are likely to be needed in South Asian countries as education and early detection will be key factors in helping curb this HF epidemic. Currently, studies report significant treatment gaps within South Asian countries. Some studies report that less than half of all people with hypertension have received a diagnosis or treatment.60,61 Even when hypertension, dyslipidaemia and diabetes are diagnosed, many government primary care facilities within this region do not carry these medications or patients must pay for these drugs out of their own pocket. This lack of resources has led to an increase in many NCDs in South Asian countries.
South Asians, both native and immigrants to many European and developed countries, are also currently vastly underrepresented in many landmark HF trials. Thus, we call that in future trials and studies that South Asians represent a major group to be investigated. Not only will this help stratify the true global impact of HF, but it may also give us a better understanding of specific ways we can target HF within the South Asian population. By emphasising the impact of HF among this population, the goal of our review article is to create significant healthcare reform changes within these countries and to begin to institute changes within these societies as controlling the impact of HF will also decrease the burden of many other NCDs.
Conclusion
Factors, such as ageing and rising populations, in many South Asian countries, alongside an increased prevalence of NCDs, point towards an impending epidemic of HF. To mediate the economic burden of HF, primary emphasis should be placed on regional and national agencies to increase awareness and improve surveillance programs. Primary preventative measures should focus on early detection of cardiovascular risk factors and optimisation of lifestyle/pharmacological management. Further studies are also warranted to directly assess the impact and prevalence of HF among South Asian descendants. Through these strategies, the goal will be to flatten the curve and enhance healthcare delivery within this region of the world.
Clinical Perspective
- South Asians are vastly underrepresented in landmark heart failure trials.
- Due to the rise in non-communicable diseases within South Asian populations, South Asian descendants are more prone to early and more advanced onset heart failure.
- Unique genetic markers have shown an increased risk of heart failure among South Asians.