The current prevalence of heart failure (HF) is estimated to be 64.3 million cases worldwide, with numbers expected to increase as the global population ages.1 Many of these individuals live with at least three additional chronic illnesses, such as diabetes, hypertension or chronic kidney disease, either as a precursor or consequence of their coexisting cardiovascular condition.2
Over the past 40 years, due to increasing patient numbers, long-term care for many patients with a chronic illness has become allocated to nurses. As a result, many nurses have taken advanced training to improve their knowledge and skills. The role and practice of the HF nurse developed from clinical studies that aimed to prevent recurrent hospital admissions for patients with HF with reduced ejection fraction (HFrEF).3,4
Current responsibilities of the HF nurse include the promotion of patient self-care, initiating and titrating evidence-based medications, being available to give prompt advice and telemonitoring support, and meeting the psychological needs of patients with a diagnosis of HF and their family members.5,6 In 2016, the European Society of Cardiology (ESC) published the HF nurse curriculum to standardise the knowledge, skills and behaviours of the nurses working in such a role so that they contribute fully to the HF multidisciplinary team (MDT).7 As a valued member of the HF MDT, these advanced nurses often work across primary and secondary care, as well as collaborating between different specialities, such as diabetology and nephrology.
Historically, most HF nurses in Europe have been based in hospital settings due to funding and governance issues.3 However, evidence shows that they can work effectively in primary or community care settings.8
Limited worldwide healthcare resources mean that many patients with HF face challenges in long-term follow-up and often have unmet physical and psychological needs. Given the global shortage of nurses, it is important to support nurses with cardiovascular expertise in developing their practice according to the needs of their service.9,10 During the COVID-19 pandemic, there was a trend towards increased reliance on digital information in the form of virtual patient consultation and digital support systems to ensure a more efficient HF service. Despite patients’ initial reluctance to embrace these changes, recent studies found many patients with HF and their caregivers recognise the benefits of the modern digital and artificial intelligence (AI) era.11,12
This integrated review of recently published evidence serves to raise awareness of the vital role the advanced or specialist HF nurse can play in early diagnosis, of treatment optimisation and strategies for effective long-term patient follow-up in the community. While this review offers a predominantly UK perspective, international evidence is integrated throughout.
Promoting Early Identification and Diagnosis
Nearly 80% of patients are diagnosed with HF during an acute hospital admission, despite over 40% having a primary care consultation because of symptoms suggestive of HF within the previous 5 years.13 To ensure timely identification and diagnosis of HF, all nurses and allied professionals working in primary care should be aware of and remain vigilant for the signs and symptoms of new (de novo) or decompensated HF at each consultation, irrespective of the patient’s presenting complaint. Working in primary care, the HF nurse has the opportunity to review data from healthy individuals, identify trends and intervene when necessary. This data may also include information obtained from digital sources, including wearable devices, such as smartwatches, health apps and fitness trackers that can monitor heart rate, activity levels and sleep patterns and provide real-time feedback.14 The information from these devices can be used by the HF nurse to promote self-management, encourage physical activity and help patients improve their adherence to recommended medication regimens.
Nurses working in primary care can develop therapeutic relationships with patients and families through routine check-ups, vaccination programmes and investigations, and this puts them in a good position to encourage patients to seek prompt treatment. There are useful checklists and infographics, for example, on the HeartFailureMatters website (www.heartfailurematters.org). In addition, the HF nurse can establish a schedule of regular teaching sessions on HF for all nurses and allied professionals in their setting, developing agreed protocols and ensuring close collaborative working between GPs and the specialist HF team.
A timely and comprehensive assessment, including interpretation of objective measurements, such as biomarker tests, completed by the HF nurse, can improve care and lead to better outcomes for patients. The serum natriuretic peptide (brain natriuretic peptide (BNP) or N-terminal proBNP (NT-proBNP)) test was given a class 1 level B recommendation in the 2021 European Society of Cardiology (ESC) heart failure guidelines.5
The UK’s National Institute for Health and Care Excellence (NICE) advocates the use of NT-proBNP measurement for suspected HF cases. For patients with very high levels (>2,000 pg/ml), NICE recommends urgent assessment of these high-risk patients within 2 weeks, while patients with levels of 400–2,000 pg/ml should be assessed within 6 weeks.15 The combination of natriuretic peptides and imaging techniques has increased the clarity of diagnosis and treatment of patients with HF with preserved ejection fraction (HFpEF).16 Many HF nurses who previously only monitored patients with HFrEF, perhaps due to funding constraints, now have a clinical requirement to broaden their remit of patients who are eligible for their care.
Many healthcare systems are looking at ways to reduce the burden of chronic disease. Although current clinical guidelines do not advocate measuring natriuretic peptides unless the patient has HF symptoms, results from the STOP-HF study highlighted the potential benefits of such testing on specific high-risk patient populations for early detection and prevention of HF-related complications.17
In Ireland, many chronic disease management clinics are either nurse- or GP-led. For example, there has been a newly funded nurse-led model of chronic disease within primary care, which provides two structured reviews annually for patients with hypertension, chronic obstructive pulmonary disease, AF, coronary artery disease and HF. In addition to education and monitoring of therapy, patients with HF have serum NT-proBNP tests assessed once a year. The specialist nurse can interpret results to identify early deterioration and reduce adverse outcomes. A recent report on the first 2 years of this model of care has shown improvements in risk factors, including a 13% reduction in smoking, 14% reduction in weight, and an improving trend in biometric measurements, such as blood pressure, LDL cholesterol and HbA1c over time.18 Nevertheless, a more strategic approach towards HF nurses working in primary care is urgently needed to guide early HF diagnosis and prompt titration of evidence-based treatments.
Post-discharge Disease Management
Digital Technology
As technology continues to advance, the integration of digital devices into HF care is expected to expand. However, this is not without challenges, be they physical problems, such as internet availability, or individual concerns, such as attitudes and preferences.19 Digital technology should not simply be a replacement for human interaction with the HF nurse and GPs. Rather, it should provide additional benefits to patients, professionals and the economy.
Digital technologies can be divided into internal/invasive sensors, such as implantable devices or pulmonary artery pressure sensors, as well as external wearable sensors and patient interfaces, such as telehealth.20 Digital and remote monitoring devices can enhance the delivery of healthcare and outcomes for patients with HF.21 In the 2021 HF guidelines, home monitoring was given a class IIb, level B recommendation; however, there remains convincing evidence in its ability to improve mortality rates and reduce hospitalisations.5,22 The HF nurse within primary care has the opportunity to educate and support the patient on the use of a specific digital device in their home.
Novel patient-focused innovations, such as those being developed by the PASSION-HF Consortium, will allow patients with HF to monitor symptoms, manage their medications and converse with a virtual doctor or nurse if required.23 This web-based AI platform can enable personalised treatment plans and interventions, enhancing patient outcomes.24 The pilot was tested in four European countries (the Netherlands, UK, Ireland and Germany), and the usability and feasibility results are pending publication. Nevertheless, it is another step towards empowering patients to self-manage their illness and thus reduce the burden placed on HF specialists, who are usually based in a hospital setting.
With the Transforming Your Health initiative in Northern Ireland and similar schemes in the rest of the UK and elsewhere, there is greater emphasis placed on patients with chronic illnesses, such as HF, to be cared for in the community.25 Such strategic initiatives support published evidence on the valuable role the HF nurse can play in primary care. For example, HF nurses reviewing patients in their own homes after they have been discharged was the most effective intervention in reducing all-cause mortality.26 Furthermore, patients who were closely monitored by HF nurses were less likely to be readmitted to hospital, with those who were admitted often discharged earlier, therefore reinforcing the cost-effectiveness of these nurses.26,27
Invasive devices, such as ICD and CRT, are well-established HF treatments, with most modern devices having the capability to wirelessly transmit data, such as congestion status and rhythm irregularities, to healthcare providers based within specialist centres to avoid the need for the patient to attend the clinic.28 HF nurses can collaborate with specialist hospital teams to adjust treatment plans and provide timely interventions in response to the data received from the patient. In addition, they can offer emotional support and reassurance to patients using digital devices, addressing any concerns or difficulties they may have.11
Telehealth platforms allow patients to attend remote consultations with their healthcare provider via a video link or telephone call and this reduces the need to travel and supports a more integrated approach to care.29 Cloud-based platforms, such as Zoom or Microsoft Teams, improve access and encourage a multidisciplinary approach to care, facilitating medication adjustments and providing education and support directly to patients.30 Despite the limitations of cloud-based technologies for patients with decompensated signs and symptoms, due to the difficulty of performing a comprehensive clinical examination remotely, newly developed AI-driven technologies offer potential for supporting objective examinations at home.31 Therefore, the HF nurse could use the platform to review patients with more stable signs and symptoms, as well as identify those patients who require an urgent in-person consultation.
In a similar format, existing digital platforms have been successfully used to facilitate shared learning between HF professionals in the hospital and the community, sharing evidence and discussing complex clinical cases. An American systematic review illustrated several quality initiatives, such as a partnership with primary care to improve overall patient care.32
Optimisation of Guideline-directed Medical Therapy
In the past decade, several randomised controlled trials have demonstrated the key role of angiotensin receptor-neprilysin inhibitors (ARNI), such as sacubitril/valsartan and sodium−glucose co-transporter-2 inhibitors (SGLT2i), such as dapagliflozin, in reducing mortality, hospitalisations, and improving quality of life for patients with HF.33,34 International guidelines recommend the four pillars of treatment, which include ARNI, β-blockers, mineralocorticoid receptor antagonist and SGLT2i for patients with HFrEF, with some divergence concerning the management of patients with HFpEF or patients with HF with improved ejection fraction (HFimpEF).5,35,36 Nevertheless, there remain concerns regarding medication inertia, with the HF nurse profiled as being part of an important strategy to counteract this.37
Initiation and titration of evidence-based medications are usually accomplished within specialist disease management clinics, due to organisational resources and governance directing service delivery. As a result, HF nurses historically have provided more of a transitional service in the community, as many were not solely employed or based within primary care. A few studies have investigated the effect of having an HF nurse based in primary care and beneficial outcomes have been reported in Sweden and Belgium.8,38 Specifically, when patients were asked their perceived satisfaction on how easy it was to contact the HF clinic in primary care, 64% were very satisfied, 29% were satisfied and 3% were dissatisfied (4% of the responses were missing).8 This indicates that for many patients, it is important to be treated close to their home as it reduces transportation costs and travel time and is, therefore, more cost-efficient and environmentally friendly.
With the publication of STRONG-HF, there has been a renewed focus on the early and quicker titration of evidence-based therapies.39 This multinational randomised trial included 1,078 patients due to be discharged following an episode of decompensation. Patients were randomised to receive maximal titration within 2 weeks of discharge and four scheduled outpatient visits over a 2-month period, or receive usual care. The trial was stopped early due to significant reductions in readmission rates and all-cause mortality in the intervention arm compared to usual care (p=0.0021). The implications of this trial were widespread, indicating an urgency for early referral and titration by a specialist HF professional, which in many European countries is now best facilitated by an HF nurse. Therefore, HF nurses working in primary care are key players in the implementation of the STRONG-HF recommendations, benefiting patients and services alike.
Patient Education and Promotion of Self-care
Recommendations within national and international guidance indicate patients with HF should participate in self-care strategies to lower their risk of clinical events and mortality.5,15 A study by Riegel et al. examined the ‘middle-range theory’ of self-care of chronic illness, identifying three core elements of self-care: maintenance, monitoring and management.40,41 These elements should be perceived as a process rather than individual activities.6 For example, maintaining healthy behaviours to improve wellbeing, monitoring or surveillance through being vigilant for changes in signs and symptoms, and management requiring continual evaluation of their HF condition and deciding on a course of action. Patient education is integral to the process and should be one of the key goals for all members of the HF multidisciplinary team.41 Nonetheless, this important task is often designated to the HF nurse either prior to discharge or during follow-up when the patient is at home.42 Information and support to monitor salt and fluid intake, as well as modifying other cardiac risk factors such as smoking, alcohol and drug use, exercise and keeping up to date with recommended vaccinations is often provided by the HF nurse. Likewise, patients should be encouraged to report a change in symptoms, for example, a new cough or change to orthopnoea, to their HF nurse or GP.
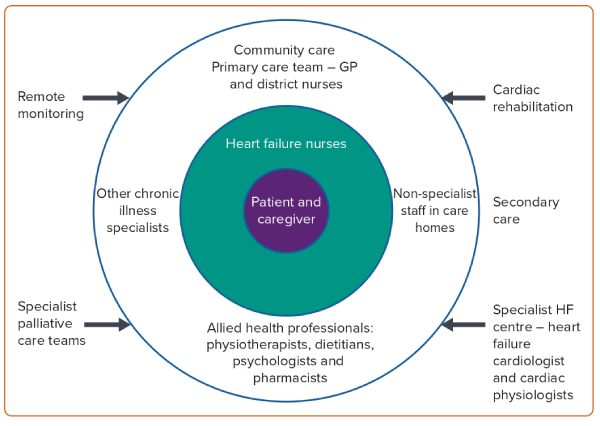
Publications by Riegel et al. highlighted the complexity of self-care and the many challenges patients with HF face, which may include a lack of family and social support, cognitive impairment and an inability to interpret change in symptoms resulting in a delay in seeking help.43,44 Following the COVID-19 pandemic, limited availability and access to many healthcare services persist.45 Waiting times have significantly increased, adversely affecting older and frailer patients with HF who may not be able to readily access specialist HF services. Integrated HF pathways aim to improve collaboration with primary care leading to earlier HF diagnosis and ultimately improved patient outcomes.46 Patients with HF, now more than ever, need to be appropriately equipped and educated about their symptoms to articulate these effectively. The HF nurse in primary care is well-positioned to support the provision of appropriate person-centred and timely care according to patient need and the availability of resources (Figure 1).
Long-term Follow-up
Provision of Non-Heart Failure Specialist Education in Community Settings
Capacity building in district or community nursing is of paramount importance if HF recognition and management are to be effectively addressed in primary care. Non-specialist nurses in these settings can play a crucial role, acting as vital links between those living at home with HF and specialist services. However, a lack of knowledge and competency in identifying HF deterioration can hinder their ability to engage with primary care providers, including the HF nurse, delaying interventions and appropriate referrals.46 To bridge this gap, targeted educational initiatives by the HF nurse should be implemented to empower non-specialists working in community settings.48
These programmes should focus on enhancing their understanding of HF signs and symptoms, improving assessment skills and facilitating effective collaboration with the HF multidisciplinary team.49 By prioritising capacity building in district or community nursing, it is possible to empower non-specialist nurses to confidently identify and manage HF, thereby improving the quality of care and patient outcomes in primary care settings.50,51
As the risk of HF increases with age, it is no surprise that the prevalence of HF in residential care homes is high, with rates between 10–45%.52–57 As such, staff within residential care homes are required to contribute to the self-care of residents with HF. However, these staff members often lack the necessary knowledge and competency to appropriately care for these residents.58 A recent scoping review of the literature encompassing 19 empirical studies revealed promising evidence supporting the effectiveness of interventions in enhancing the care of residents with HF within care home settings. These findings highlight the crucial role of staff education and access to HF specialists, such as the HF nurse, as key factors for achieving successful outcomes.59 Further research is needed to ascertain the impact of such interventions on the quality of life and long-term care provision for care home residents with HF.
Palliative Care
After examining community nursing and care homes, it becomes crucial to address the topic of palliative care. Community palliative care services for patients with HF throughout Europe are the exception, not the norm. International studies, using a variety of interventions, professionals and settings, have demonstrated the benefits of integrating a palliative care approach into the management of patients with HF.60–63 Despite such evidence, heterogeneity across studies has led to limited progression, further reinforced by inherent discrepancies between the recent US and European HF guidelines.5,35
Community palliative care for patients with HF remains the remit of GPs and district nurses, who can manage non-complex palliative symptoms, and clarify and record patients’ and caregivers’ expectations and goals of treatment. Evidence is sparse. However, a sustainable and cost-effective model may be the upskilling of HF nurses to support palliative care in the community and thus reduce the rates of referral to specialist primary care teams.64,65 Recent position papers have documented the importance of upskilling both palliative and HF professionals through shared learning, to improve collaborative working.66,67
Many patients would prefer to be cared for at the end of life within their own homes. This often requires the nurse to navigate organisational, cultural and resource challenges. The HF nurse can facilitate this through the therapeutic relationship they have developed with the patient and their family, as well as the communication and collaboration with interdisciplinary professionals, including pharmacists and physiotherapists.68
Patient Perspectives
Recent evidence showed three key themes regarding the patients’ perspectives of HF care within the community setting. Effective communication and patient education were highly valued, with patients seeking clear explanations of their diagnosis, treatment options and self-care strategies in clear and understandable language that was free of jargon.6 Continuity of care was also important, with patients desiring a primary care provider who knew their medical history, understood their unique needs and could coordinate their care effectively.69 Access and timeliness of care were emphasised, with patients valuing access and prompt attention from their primary care provider, with consistent and seamless transitions between healthcare settings. These three themes are more likely to be achieved for patients when the service involves an HF nurse in primary care.
A holistic approach to HF care was desired, provided close to home and addressing not only physical aspects but also emotional and psychosocial needs.70,71 Patients with multimorbidity often travel to and consult with a number of specialists, each focusing on a specific condition, leading to difficulties in harmonising and adherence to complex treatment regimens.72–74 Many visits and therapies result in patients and their families/caregivers experiencing an undue burden of treatment.74 Family members can provide support, assist with medication adherence, encourage lifestyle modifications, and help monitor symptoms. Their crucial involvement helps create a conducive environment for patients to thrive and enhances the overall quality of care they receive.74 The nurse can support the needs of the patient and caregiver throughout the HF journey.
Limitations
This pragmatic review has some limitations. First, many articles refer to the ‘HF nurse’ and do not specify the location of their practice, be that solely within a community setting, hospital setting or both. Rather, there is more published evidence regarding the role of the HF nurse in the transition of the patient to the community. Second, there is recognised heterogeneity in the role and practice of HF nurses across Europe, which requires further research.
Conclusion
Many patients prefer to be cared for close to home in a familiar setting. HF nurses have the potential to play an important role in delivering patient-centred care to patients with HF and their caregivers. By collaborating across geographical and speciality boundaries and incorporating new digital technologies and ways of working, HF nurses can improve patient outcomes. However, there is a need for a clear educational pathway to align with the expanding role and practice of community-based HF nurses across Europe and beyond.