Heart failure remains a significant burden to the US healthcare system and contributes greatly to the morbidity and mortality of the population. The impact of an ageing population, improved survival in coronary artery disease (CAD) and adverse life-style choices will ultimately result in an increased burden on an already taxed health care system.
Heart failure affects over 5 million people with approximately 550,000 new cases every year.1 While the prevalence of heart failure is significantly higher in the older population (>65 years), 1.4 million patients <60 years of age carry the diagnosis of heart failure. The estimated $32 billion cost of heart failure is due in large part to the more than 1 million hospital admissions for acute care. Following the first admission for acute decompensated heart failure (ADHF) the readmission rates are nearly 50 % at six months and mortality reaches 30 % at 1 year.2,3 The short-term risk of readmission remains unacceptably high, 15 % at 60 days and 30 % at 90 days. Unfortunately even with all of the advances in medical therapy the post-admission morbidity and mortality has not been significantly reduced. As with most chronic illness, the impact of co-morbidities adversely affects the outcomes in heart failure.
Diabetes mellitus (DM) has been shown to be a significant risk factor for the development of heart failure and negatively impacts the prognosis. Over the past two decades the prevalence of diabetes has sharply increased from 3.5 % in the 1990s to greater than 9 % in 2012.4 Diabetes impacts the lives of nearly 30 million Americans and by the age of 65 nearly one quarter of the population carries the diagnosis. The cost of DM to the health care system is nearly $250 billion, with close to $175 billion in direct costs.5
Traditionally the two illnesses have been managed in relative isolation. However with the high incidence of the co-existence of these two chronic diseases, especially as the prevalence of both continue to grow, clinicians should be more cognisant of the impact each has on the other.
The Epidemiology of Heart Failure in Diabetes Mellitus
The increased incidence of heart failure in diabetics was first described in the Framingham Heart Study. In the original publication, DM conferred twice the risk in men and nearly five times the risk in women for the development of heart failure.6 Since then the impact of DM on the incidence of heart failure has been repeatedly demonstrated. The incidence of heart failure is 2.5 times higher in diabetics than the general population.7 Diabetes contributes not only to the increased incidence of heart failure, but it is also an independent risk factor for left ventricular hypertrophy, a clearly defined precursor to heart failure.
In the Cardiovascular Health Study, diabetes was shown to be an independent risk factor for the development of heart failure.8 The increased risk for the development of heart failure is magnified in two specific sub-populations. As the diabetic population ages the risk of developing heart failure increases. Demonstrated in a Kaiser Permanente registry the incidence of heart failure doubles in diabetics for every decade above 45 years of age9 and similarly in a study of the elderly (>65 years), 39 % of diabetic patients developed heart failure compared to 23 % of non-diabetics after 3.5 years.10 In a study of 150,000 Medicare patients the incidence of heart failure was 13 % and the prevalence reached 24 %.11 Patients with a history of ischaemic heart disease and diabetes are also at increased risk for the development of heart failure compared to those without an ischaemic burden. Tenebaum A et al. demonstrated that heart failure developed more frequently in DM with ischaemic heart disease compared to those with non-ischaemic heart disease, 46 % vs 36 % respectively. Even the presence of impaired fasting glucose in ischaemic heart disease carried an increased risk of heart failure.12
While the diagnosis of diabetes is an independent risk factor for heart failure, recent data has shown that glycaemic control is an important prognostic marker for heart failure. Glycosylated haemoglobin (HgbA1c) is directly associated with the risk of heart failure. An increase in HgbA1c from 6.5 % to 10.5 % increases the risk of developing heart failure nearly 4-fold.13 The risk of heart failure increases linearly with increasing HgbA1c. For each 1 % increase in HgbA1c the risk of heart failure increase 8–12%.14,15 The risk for the development of heart failure in diabetics may be more closely related to overall long-term glycaemic control and duration of DM, rather than the HgbA1c at an individual point in time.
The Epidemiology of Diabetes Mellitus in Heart Failure
Patients with heart failure demonstrate impaired glucose metabolism and insulin resistance is common.16 The altered glucose metabolism places them at increased risk for developing diabetes, 29 % vs 18 %, compared to the general population.17 Data from multiple randomised studies and registries agree that the prevalence ranges from 20 %18 to 26 %.19 In fact nearly one quarter of all HF patients have concomitant diabetes and this number rises drastically to 40 % in patients admitted with ADHF.20 In the SOLVD (Studies of Left Ventricular Dysfunction) trial 6 % of patients developed DM within three years of enrollment.17 The overall prevalence of DM in heart failure is significantly higher than in the general population, 25 % compared to 9 %. While the overall prevalence of DM is 25 % in heart failure, patients with Heart Failure with Preserved Ejection Fraction (HFpEF) have a slightly higher prevalence of DM reaching nearly 40 %.21
Outcomes in Heart Failure with Concomitant Diabetes
The co-existence of heart failure and diabetes has significant impact on outcomes and confers a worse prognosis than heart failure alone.22 The diagnosis of diabetes in heart failure patients results in increased cardiovascular mortality, higher readmission rates23 and increased hospital lengths of stay.24 Data from ALLHAT (The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial) demonstrated significantly higher risk for heart failure admissions or death in diabetics, nearly twice as high than in those patients without diabetes.25 The presence of diabetes in heart failure confers a significantly higher rate of mortality compared to those without diabetes, 45 % versus 24 % respectively, at 5 years.11
The poor prognosis of concomitant DM and HF is more prominent in two sub-groups of patients with heart failure. The SOLVD trial showed an increased risk for HF admissions (RR:2.16) or a composite of death or symptoms in HF (RR:1.56) in patients with asymptomatic ischaemic cardiomyopathy26 and in the Framingham Heart Study 34 % of diabetic patients died within 1 year of the diagnosis of heart failure.27 The other sub-group of heart failure patients that experience worse outcomes
with DM are patients with HFpEF. As previously demonstrated, patients with HFpEF have a higher prevalence of DM. In the CHARM (Candesartan in Heart Failure: Assessment of Reduction in Morbidity and mortality) study patients with HFpEF and concomitant diabetes had higher rates of CV death and hospitalisations for heart failure compared to those with reduced EF.28
As was previously shown HgbA1c is directly related to the risk of developing heart failure. It has also been demonstrated that it directly impacts outcome in heart failure. In heart failure, the effect of HgbA1c on morality is U-shaped. Morality decreases with decreasing glycosylated haemoglobin until a nadir is reached, then the mortality begins to creep upwards again. The highest mortality is seen in patients with HgbA1c > 7.8 % and < 7.1 %,indicating that the optimal HgbA1c goal in DM to reduce the risk of death in heart failure is approximately 7.5 %.29 Glycaemic control has been thought to be paramount to reducing the risk and impact of DM on the development and prognosis of heart failure. Achieving adequate glycaemic control requires the use of hypoglycaemic agents and often exogenous insulin. However therapies utilised to improve glycaemic control are often a double-edged sword, especially in heart failure. Randomised controlled trials have failed to show a benefit of tighter glycaemic control on the incidence of heart failure.30,31 The use of insulin in heart failure is controversial, while excellent glycaemic control can be achieved, it has been associated with increased mortality in HF.32 The use of metformin is cautioned due to the increased risk of metabolic acidosis and is not recommended in advanced heart failure. Trials with thiazolidinediones (pioglitazone and rosiglitazone) have demonstrated adverse outcomes in heart failure, increasing the risk of heart failure and hospitalisations by nearly 2-fold.33,34 It is thought that these medicines promote fluid retention and alter sodium handling resulting in worsening heart failure. In a recent analysis of the dipeptidyl peptidase-4 (DPP-4) inhibitor saxagliptin its use was associated with a significant increase in heart failure admissions.35 Sulfonylureas, which increase endogenous insulin production, have not been shown to negatively impact the development of heart failure. Clearly the optimal therapeutic strategy remains elusive.
Conclusion
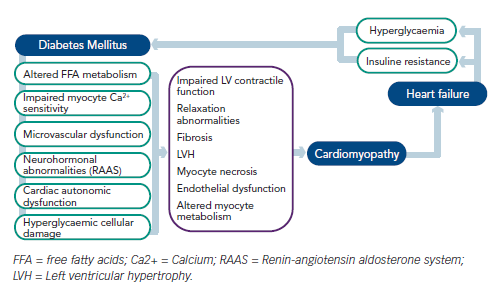
Data presented here demonstrates that these two chronic comorbid conditions cannot be thought of as two separate and distinct entities, nor can they be treated in isolation. Diabetes affects myocardial glucose metabolism, cardiac fatty acid metabolism, intra-cellular calcium cycling, accelerates coronary artery disease, contributes to microvascular dysfunction, neurohormonal upregulation and increases cardiac fibrosis.20 The combination of these pathophysiological abnormalities increases the risk for developing heart failure and place added strain on an already taxed myocardium. Patients with heart failure have altered glucose metabolism and high rates of insulin resistance, increasing the risk for the development of DM. This bi-directional impact on the other disease process inexorably links these to chronic conditions together (see Figure 1). The combination of heart failure and diabetes mellitus portends worse prognosis than either comorbidity alone.
As the population of developed countries ages and the sedentary life-style, obesity rates and prevalence of hypertension increase, the prevalence of heart failure and diabetes will continue to grow. Therapies, both non-pharmacological and pharmacological, must focus on both the prevention of these devastating illnesses and on reducing their combined impact on morbidity and mortality in the population. Future research is required to address the risk and benefit of therapies directed towards each individual disease to reduce the impact on the other.